Intracranial pressure
(Redirected from Increased intracranial pressure)
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Intracranial pressure | |
|---|---|
| |
| Synonyms | ICP |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Headache, vomiting, altered mental status, papilledema |
| Complications | Brain herniation, cerebral ischemia, death |
| Onset | Sudden or gradual |
| Duration | Variable |
| Types | N/A |
| Causes | Traumatic brain injury, stroke, brain tumor, hydrocephalus, meningitis |
| Risks | Hypertension, coagulopathy, infection |
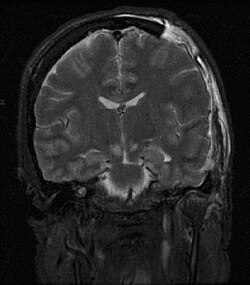
| Diagnosis | Clinical examination, CT scan, MRI, lumbar puncture |
| Differential diagnosis | Migraine, tension headache, subarachnoid hemorrhage |
| Prevention | N/A |
| Treatment | Osmotic therapy, surgical decompression, ventricular drain |
| Medication | Mannitol, hypertonic saline, corticosteroids |
| Prognosis | Depends on cause and treatment |
| Frequency | Common in intensive care unit settings |
| Deaths | N/A |
Intracranial pressure (ICP) is the pressure within the cranial cavity, the space inside the skull where the brain resides. This pressure is influenced by the volume of three main components: brain tissue, cerebrospinal fluid, and blood. Normal ICP ranges from 5 to 15 mmHg in a supine adult. Alterations in ICP can have profound effects on cerebral physiology, leading to serious complications or even death if not addressed promptly.
Understanding Intracranial Pressure
The balance between the production and absorption of cerebrospinal fluid (CSF) and the blood flow to the brain primarily governs ICP. This delicate balance is guided by the Monro-Kellie doctrine, which postulates that the total volume of blood, CSF, and brain tissue remains constant in the rigid skull. Any increase in one of these components necessitates a decrease in one or both of the other two to maintain a normal ICP.[1]
Physiological Variations and Measurement of Intracranial Pressure
ICP can vary physiologically due to changes in body position, respiration, and arterial pressure. However, pathological elevations or reductions in ICP can lead to serious health issues, including stroke, traumatic brain injury, hydrocephalus, or brain tumors.[2] Measuring ICP is crucial in the diagnosis and management of these conditions. Direct invasive methods like ventriculostomy or intraparenchymal monitoring are the gold standard for accurate ICP measurement, although non-invasive methods are under development.[3]
Consequences of Altered Intracranial Pressure
When ICP is either excessively high or low, it can lead to severe neurological impairment and may become life-threatening. Increased ICP can reduce cerebral blood flow, resulting in brain ischemia and neuronal death. In contrast, decreased ICP, though less common, can lead to conditions such as spontaneous intracranial hypotension, characterized by postural headaches.[4]
Treatment Strategies for Abnormal Intracranial Pressure
The management of abnormal ICP is a critical aspect of neurocritical care. Treatment strategies for elevated ICP include sedation, hyperventilation, osmotherapy (using osmotic diuretics such as mannitol), and surgical interventions like decompressive craniectomy. On the other hand, treatments for low ICP typically involve addressing the underlying cause, such as repairing CSF leaks.[5]
Conclusion
In conclusion, intracranial pressure plays a pivotal role in maintaining brain health. Careful monitoring and management of ICP are key to preventing and treating various neurological disorders.
References
- ↑ , The Monro-Kellie hypothesis: applications in CSF volume depletion, Neurology, 2001, Vol. 56(Issue: 12), pp. 1746–1748, DOI: 10.1212/wnl.56.12.1746, PMID: 11425944,
- ↑ , Measuring elevated intracranial pressure through noninvasive methods: a review of the literature, Journal of Neurosurgical Anesthesiology, 2013, Vol. 25(Issue: 4), pp. 372–385, DOI: 10.1097/ANA.0b013e318293f5c2, PMID: 23872804,
- ↑ , Accuracy in the measurement of intracranial pressure: systematic review and meta-analysis, Journal of Neurosurgery, 2019, Vol. 132(Issue: 5), pp. 1479–1494, DOI: 10.3171/2019.2.JNS182507, PMID: 31125970,
- ↑ , Spontaneous low pressure, low CSF volume headaches: spontaneous CSF leaks, Headache, 2013, Vol. 53(Issue: 7), pp. 1034–1053, DOI: 10.1111/head.12149, PMID: 23808994,
- ↑ , Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition, Neurosurgery, 2017, Vol. 80(Issue: 1), pp. 6–15, DOI: 10.1227/NEU.0000000000001432, PMID: 27654000,
See Also
- Monro-Kellie doctrine
- Cerebral blood flow
- Brain ischemia
- Spontaneous intracranial hypotension
- Neurocritical care
| This article is a medical stub. You can help WikiMD by expanding it! | |
|---|---|
| Physiology of the nervous system | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Diseases of the nervous system, primarily CNS (G04–G47, 323–349) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Transform your life with W8MD's budget GLP-1 injections from $125.
W8MD offers a medical weight loss program to lose weight in Philadelphia. Our physician-supervised medical weight loss provides:
- Most insurances accepted or discounted self-pay rates. We will obtain insurance prior authorizations if needed.
- Generic GLP1 weight loss injections from $125 for the starting dose.
- Also offer prescription weight loss medications including Phentermine, Qsymia, Diethylpropion, Contrave etc.
NYC weight loss doctor appointments
Start your NYC weight loss journey today at our NYC medical weight loss and Philadelphia medical weight loss clinics.
- Call 718-946-5500 to lose weight in NYC or for medical weight loss in Philadelphia 215-676-2334.
- Tags:NYC medical weight loss, Philadelphia lose weight Zepbound NYC, Budget GLP1 weight loss injections, Wegovy Philadelphia, Wegovy NYC, Philadelphia medical weight loss, Brookly weight loss and Wegovy NYC
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD


